What is the difference between Optic Nerve Hypoplasia and Septo Optic Dysplasia?
A child with Optic Nerve Hypoplasia has optic nerves that are small and poorly developed. Instead of having over 1 million connections (nerve fibers) from each eye to the brain, people with Optic Nerve Hypoplasia have far fewer connections. The more connections between the eye and the brain the better the vision. Some people with Optic Nerve Hypoplasia have near normal vision in one eye, others have decreased vision in both eyes, and others are severely affected and nearly blind. An eye doctor (Ophthalmologist) can diagnose ONH by looking inside the eye with an ophthalmoscope. The front surface of the optic nerve (optic disc) appears smaller than normal. Most people with ONH have a nystagmus (unusual eye movements). The eyes may seem to move around with no real pattern or purpose. This occurs because the eyes are not able to focus well enough to hold still.
Typically people with Septo Optic Dysplasia have abnormalities of the brain. These abnormalities may include how the brain is formed (brain structure) and how the brain works (brain function). While both usually occur, sometimes a child has a problem only with the structure of the brain and at other times, a child has a problem only with the function of the brain. All problems with the brain can range from mild to very serious. When a child is diagnosed with Septo Optic Dysplasia he or she will undergo a number of evaluations and brain function tests (neurologic tests). A brain specialist (Neurologist) can look at the brain structure through the use of CT (computerized tomography) or MRI (magnetic resonance imaging). After these tests are performed your doctor should be able to tell if there are major problems with the brain structure.
Septo Optic Dysplasia Predictions
Doctors cannot always predict if a child will or will not have problems with brain function. When a child is less than 3-4 years of age, it is often difficult to predict future brain functions such as speech, intelligence and learning. It is sometimes difficult to assess the brain function and overall development of a child with poor vision. Visually impaired children must be taught and tested in ways that are different than children who are not visually impaired. Be sure that your child is tested and treated by professionals who have experience working with children with poor vision. Testing to determine how you child is developing and to screen for learning problems can be done by specialists such as: pediatricians, psychologists, occupational therapists (OT's), speech therapists (SP's), physical therapists (PT's) and teachers of the visually impaired (VI's). Testing can be done in several different settings including your own home, schools, hospitals, or other clinical settings.
Pituitary effects for Septo Optic Dysplasia
The pituitary gland is found at the base of the brain and serves as the body's "master control gland" because it makes important chemicals (hormones) and directs the making of hormones in glands located in other parts of the body. These hormones are required for growth, energy control (metabolism) and sexual development. Many people with Septo Optic Dysplasia have problems with their pituitary gland ranging from very minor problems with almost no effect on the child, to problems making one or more very important hormones. When a child has problems making hormones in the pituitary gland it is called hypopituitarism. Your child will be tested to see if there are any problems making hormones. A doctor who specializes in gland problems (an Endocrinologist) will order tests to be done at the time of diagnosis. A child who initially does not have hormone problems may develop them at a later time. Therefore, it is very important for your child to be tested regularly as he or she grows up.
The pituitary produces a hormone called Anti-diuretic Hormone (ADH) that is responsible for keeping water in the body by controlling the amount of urine (pee) that is created. Without enough ADH a person cannot control the amount of urine and he or she loses too much water from the body (becomes dehydrated). The person feels very thirsty, has a dry mouth and yet continues to make large amounts of urine. If the child cannot get enough fluid to replace what is being lost in the urine, this can lead to dehydration and a very high level of sodium (a mineral) in the body. This dehydration can cause serious problems. If this problem is suspected, your child may need to have blood and urine tests. Sometimes a special test called a water deprivation test needs to be done. This involves a test lasting up to 8 hours which is done in the hospital or specially equipped office. Your child will not be able to have anything to drink for the entire test. Blood and urine tests are done to see if the proper amount of ADH is being created. If your child does not make enough ADH (called Diabetes Insipidus [DI] or water diabetes), treatment is available. The most common treatment is a medicine called DDAVP. It can be given in the nose, by mouth, or by injection.
Growth Hormone and Septo Optic Dysplasia
Growth hormone (GH) is made in the pituitary gland and controls the growth of the bones. Lack of growth hormone causes a child to grow at a slower than normal rate. Some children who lack growth hormone also have low blood sugar. Without treatment, your child will be shorter than expected when growth is finished.
With proper treatment you can expect your child's growth to be close to what it would have been without a growth hormone problem. About 6 in 10 children with ONH do not make enough growth hormone.
Cortisol and Septo Optic Dysplasia
Cortisol is made by the two adrenal glands located on both sides of the middle of the back above the kidneys. A hormone from the pituitary gland (ACTH) signals the adrenal gland to make small amounts of cortisol at various times during the day. Cortisol is also made during times of physical stress (such as during surgery, when suffering from an illness or injury, or when the body is dehydrated). The extra cortisol is necessary to help the body continue to create energy, control the blood sugar and allow for proper heart and lung function. The normal pituitary gland signals the adrenal gland during these periods of stress to make extra cortisol. Your child should have blood tests to see if he or she is able to make enough cortisol. If the level is found to be low, some children will need special tests (called cortisol stimulation tests) to find out if they make some cortisol or if they are not able to make any cortisol. If your child is found not to make enough cortisol, he or she may need to take a cortisol replacement medication by mouth 1 or 2 times each day. Additional cortisol might also be necessary during times of physical stress. If your child has problems with cortisol, you should get additional information about caring for a child with this problem.
Thyroid Function and Septo Optic Dysplasia
Thyroid hormone is made by the thyroid gland in the neck. With a poorly functioning pituitary gland, the thyroid gland does not get the proper signal (TSH) to make thyroid hormone when it is needed and the person does not make enough thyroid hormone (hypothyroid). Thyroid hormone helps in normal growth and helps make energy for the body to function (metabolism). Lack of thyroid hormone can lead to poor growth, slowing of mental and muscle function, weight gain, feeling cold, irregular periods (menstrual cycle), hair loss, hoarse voice, brittle nails, and dry coarse skin. Lack of thyroid hormone can be shown with blood tests. The main thyroid hormone measured is called thyroxine (or T-4). Thyroid hormone levels should be checked when the diagnosis of Septo Optic Dysplasia/Optic Nerve Hypoplasia is made. If your child lacks thyroid hormone, he or she can easily be treated with thyroid pills taken by mouth every day. Your child will need to have T-4 measured regularly to see if the right amount of medicine is being given. With proper treatment, your child's thyroid problem will be corrected and he or she will not suffer ill effects.
A Personal Story
 My name is Krystal. I am a mom to five. My son Keegan has Septo-Optic Dysplasia. I am married to an amazing man. I am the founder of A Blind Journey. I am mom on a mission to share hope and raise awareness for children with special needs. I am jokingly known as the next Martha Stewart. I love being a mother and a wife. I recognize that I live a very blessed life. I am honored to join MAGIC and look forward to being part of an amazing team of people!
My name is Krystal. I am a mom to five. My son Keegan has Septo-Optic Dysplasia. I am married to an amazing man. I am the founder of A Blind Journey. I am mom on a mission to share hope and raise awareness for children with special needs. I am jokingly known as the next Martha Stewart. I love being a mother and a wife. I recognize that I live a very blessed life. I am honored to join MAGIC and look forward to being part of an amazing team of people!
The road leading to where I am today is not what someone looking in would expect. I’ve spent a long time lost, confused, and alone (or at least I felt alone). I guess that is why it is difficult to write about, which I sometimes refer to as a lifetime ago. I feel everything as if it was yesterday but I am no longer the girl I was then. Too much has happened, and I don’t spend much time looking back. Many of you have experienced something similar. One thing I know is that we are guaranteed pain and disappointment in this life. The only thing that got me through those days is knowing that everything happens for a reason. The silver lining? I have grown in ways I never knew possible, including my shattered heart.
My sweet Keegan was born in June of 2006. My pregnancy was kind of a mess, well not my pregnancy so much as my doctor. During an ultrasound, I was informed that it looked like there was a lack of fluid in my placenta and what appeared to be extra fluid in the brain. I was told not to worry, they would monitor me more closely with stress tests, and have orders for the baby to have more tests and see a neurosurgeon at birth. He would probably need a shunt to drain the excess fluid. I spent the remainder of my pregnancy listening to his heartbeat twice a week. Everything else was fine; there were no concerns from any of the latter visits. I spoke with the woman that was to be his pediatrician and she assured me that it was probably nothing. She said that the OB wasn’t overly concerned and I should not be either, it would likely be nothing at all.
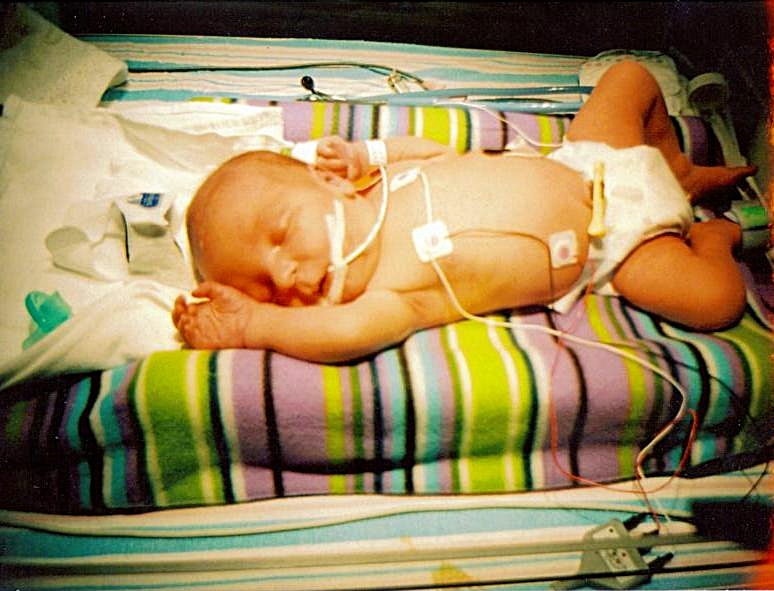
I was induced a week early so as not to add any undue stress to the baby by passing my due date. Labor was a breeze, if you don’t account for the fact that induction is literally birth on steroids (OUCH!). Hooray for an effective epidural! Except that post-delivery was a little hazy. It’s a boy. I thought aw man, I was really hoping for a girl! I held him for a moment, before they took him. I woke up at some point and Keegan’s father told me they took Keegan to be monitored because he was having some trouble breathing. He said something about suctioning his nose, causing some irritation, no big deal. Later he told me that Keegan was whisked away to the NICU and that he was secretly terrified and didn’t want to worry me. My baby never did come back to my room.

Once I was able to walk, I went to see him in the NICU for the first time. Seeing my baby in a box, hooked up to monitors, tubes and wires. Scrubbing my arms with iodine and putting on a paper gown. Not being allowed to hold him. Not being allowed to breastfeed him. I didn’t know how to react. I don’t remember how I reacted. I think everything just shut off. I looked around at all of the other little babies in that room, my heart ached for every one for their families. I went back as often as I was allowed. The hospital allowed me to stay another day even though I could be discharged. Keegan was breathing better. He wasn’t eating enough, and had to have a tube in his nose. That bothered me. He was jaundiced. I still thought that everything could be okay. After 3 days, a sweet woman asked to meet with us and told us that Keegan saw a myriad of different doctors, had an MRI, and blood work and that he had Septo-Optic Dysplasia. She explained what is was, that he needed hormone replacement, his vision might be affected but it would be a while before we could tell. She was very encouraging. I remember taking the news as if it were orders for battle. Keegan’s dad began to crumble. Harder than hearing the diagnosis was leaving the maternity ward without my baby. Nobody knew how long he would be there.
This time I wouldn’t be rolled out in a wheelchair holding my baby. I would have to watch countless other mom’s as I visited the hospital multiple times a day taking their babies home, while I went to scrub my skin with iodine and look at my baby in a box being force fed via a tube down his throat. I had to hold it together. Keegan’s lack of appetite was the one thing holding him in the NICU.
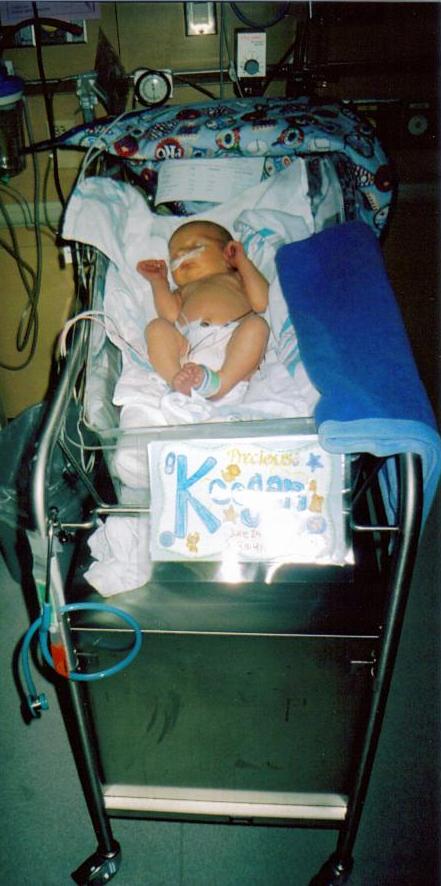
The very day Keegan was scheduled for surgery to have a g-tube the endocrinologist put on the brakes . Results from his blood work showed he was growth hormone deficient. She believed once he had growth hormone replacement he would eat better. It would take a little while to get the medication, and I would have to be trained to give my infant an injection but she was insistent we wait to have surgery. At that point, I would have walked across hot coals and broken glass to bring my baby home. I learned to give Keegan his GH shot and taught all of the nurses in the NICU as well. I was there every night to give it to him. After four long weeks, we finally freed Keegan! With his growth hormone levels within normal range, he was eating enough to take the wretched tube out of his nose and go home! I practically ran out the doors afraid they would change their minds.
In those four weeks, my entire life turned upside down. I did not have a baby girl to name Isabella. My baby was not okay. I became a single mother after some utterly terrifying events. Nobody could tell me with any certainty what my future would hold. A week after Keegan was released I moved across the state to live with my mom and step-dad, looking for a fresh-start and desperately needed support.
Looking back over the last six years, there were some very dark times. What kept me going was that when things got hard I fought harder. I may not have had much hope, that didn’t come until later. I didn’t really reach out for help, I had to learn how to do that. I found MAGIC and joined the Yahoo group. I posted a handful of times and would periodically read what others wrote. Then I would pull back, I still felt detached. The first three years of Keegan’s life were a huge learning curve. We spent a minimum of one week out of every month hospitalized. Every illness had the potential to become life threatening at the drop of a hat.

Then there were the “episodes.” Something switched and my mellow quiet baby became a screamer. He would have episodes where he would gasp and tense up, his eyes would roll up, and then it would release and he would scream. This would repeat for up to 10 minutes. It would happen sporadically throughout the day and night, it was always worst at night. Nothing would soothe him, not even the Tylenol with codeine for his “ear infection.” I would lay him down and curl up in a ball and sob until it was done. Then, as quickly as it started, it would stop. Keegan would take a bottle and drift away. I knew it was seizures, I said it a dozen times. I wanted so badly to be wrong, and an ear infection sounded much better. A week and a half later and the “ear infection” wasn’t getting any better.
I went to see our pediatrician this time and while we were waiting, he had another episode. I called the nurse in, she took one look at him and her face gave her away. Something was seriously wrong. She left to speak with the doctor. He came in and said that he was ordering an EEG; we would have to go to the next town to have it done. He wanted us to see a neurologist 2 hours away. They would probably have a waiting list. He hoped that getting an EEG done would help speed up the process.
I went to see this neurologist the day before Keegan’s first birthday and he told me what I already knew: He was having seizures. A very serious, difficult to control, and damaging kind. Keegan was hospitalized so that they could do more tests and start treatment right away. The only saving grace is that our Neurologist was amazing. He had the task of delivering the worst news to date to an already fragile mom and he did it well. He was kind and respectful, he explained everything clearly, and he was a father and gave me his honest opinion. He involved me in every decision for new medications to try. He told me the facts in a way that didn’t leave me defeated. Trust me during that time there were plenty to try to steal the little sliver of hope I had left. After many long months there was a day that I noticed Keegan didn’t have a seizure. We had another EEG and the hypsarrhythmia pattern was no longer present, and eventually we were declared seizure free!

Fast forward a few years to today. My crazy haired, doe eyed Keegan is in first grade. He is considered to be on the severe end of the SOD/ONH spectrum. We are told he is completely blind, I will accept that when he is able to tell me himself. He attends a school for children with special needs, where he gets to go swimming and ride horses every week. Keegan receives PT, OT, and Speech in school as well as out. He also receives ABA therapy in which he is learning to scoop and take bites himself, among other things. On Monday, he begins his second round of Intensive Physical Therapy. We hope that he will continue to make developmental gains; his therapist believes that one day he will be able to walk. I continue to fight to help him achieve his full potential. That is just a glimpse into our story; you are welcome to read more on my blog: www.ablindjourney.com
Contributing Medical Specialist
Francine R. Kauffman, MD
Endocrinology & Metabolism Director
Comprehensive Childhood Diabetes Center
Children's Hospital, Los Angeles, California
Neal Kauffman, MD, M.P.H.
Director, Division of Academic Primary Care Pediatrics
Cedars-Sinai Medical Center
Professor of Pediatrics and Public Health
UCLA Schools of Medicine and Public Health